Understanding Mental Health CPT Codes for Accurate Billing
Mental health CPT codes form the backbone of therapy billing. Every therapy session, evaluation, or psychiatric service must be assigned the correct CPT code to ensure clean claims and timely reimbursement. If providers apply the wrong code, mismatch session duration, or fail to document correctly, insurers reject the claim on the spot. That’s why mental health CPT codes must be accurate, consistent, and aligned with payer rules from the beginning.
Private practices often deal with denied claims because they don’t follow time-based coding rules, documentation standards, or code updates. Without mastering mental health CPT codes, your revenue cycle collapses. A clean claim depends entirely on using the correct code for the exact session type and time spent — nothing else matters more.
Commonly Used Mental Health CPT Codes and Their Importance
Standard Psychotherapy CPT Codes
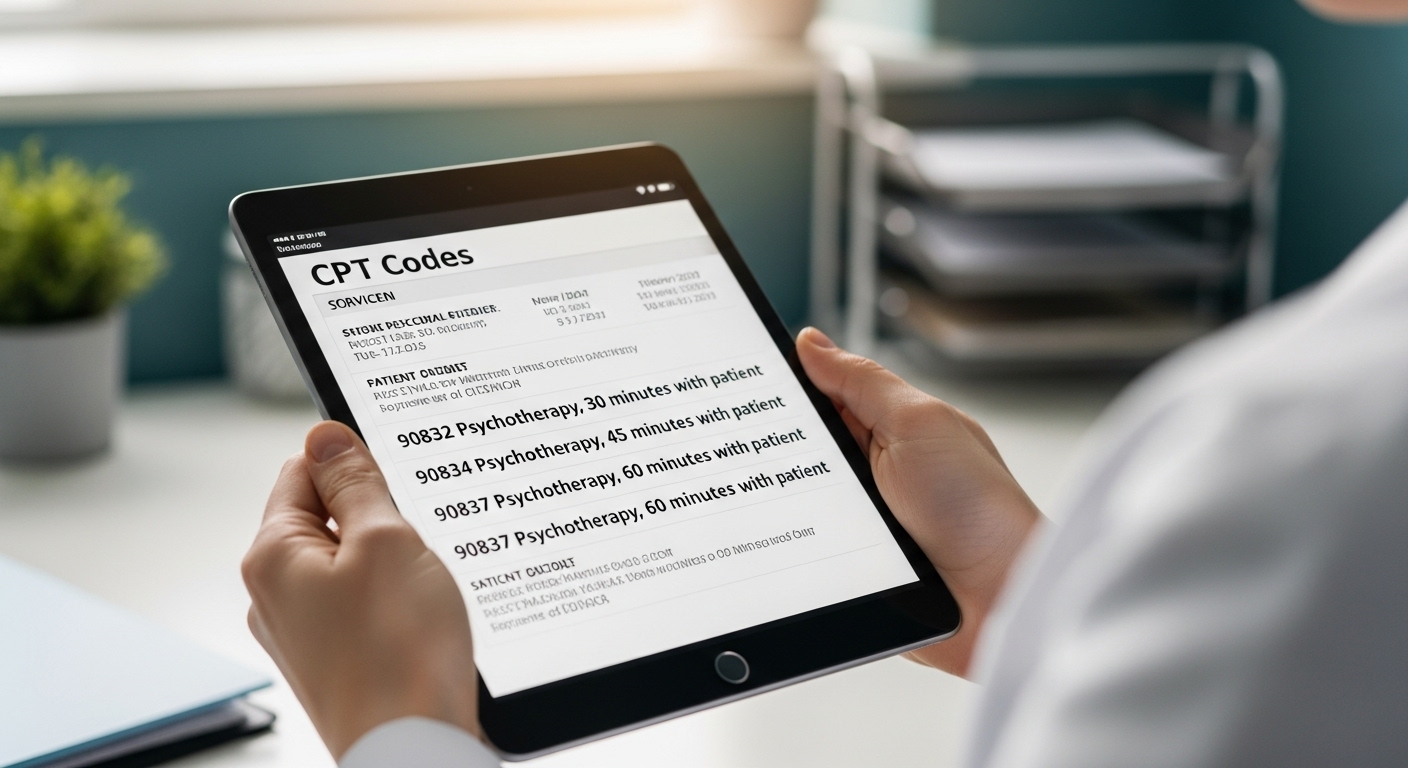
These codes are the core of mental health billing. They represent different therapy session durations:
- 90832 – 30-minute psychotherapy
- 90834 – 45-minute psychotherapy
- 90837 – 60-minute psychotherapy
Most claim denials occur because the provider’s documentation does not match these time requirements. If your notes don’t confirm the exact session length, insurers downgrade or deny the claim.
Add-On Codes for Extra Time
Some sessions require more time than usual. CPT code +90840 is used as an add-on when psychotherapy is extended. Practices that skip add-on codes lose money simply because they underbill.
Psychiatric Diagnostic Evaluation Codes
These codes cover initial assessments, history-taking, and mental health evaluations:
- 90791 – diagnostic evaluation without medical services
- 90792 – diagnostic evaluation with medical services
Using the wrong code here means the provider either gets underpaid or denied because the service doesn’t match payer expectations.
CPT Codes for Psychiatric Medication Management
Psychiatrists and psychiatric nurse practitioners rely on medication management codes:
- 99213 and 99214 – evaluation and management with varying complexity
- 90863 – add-on code for pharmacologic management
Errors happen when providers bill only E/M codes and forget to add 90863, losing revenue they earned.
CPT Codes for Group and Family Therapy
Mental health care extends beyond individual therapy. Insurance companies require specific codes for non-individual sessions:
- 90846 – family therapy without patient
- 90847 – family therapy with patient present
- 90853 – group therapy session
Providers who treat couples, families, or groups must use the correct CPT code or risk denials for “incorrect session type.”
Telehealth CPT Codes for Mental Health Services
Telehealth billing rules change constantly, and many practices still get them wrong. Most virtual psychotherapy codes mirror in-person services, but require telehealth modifiers. Standard mental health telehealth CPT codes include:
- 90832, 90834, 90837 – psychotherapy via telehealth
- 90791, 90792 – telehealth diagnostic evaluation
Payers often require modifiers like 95 or GT, and using the wrong one triggers automatic denial. Telehealth services also require correct POS codes (typically POS 10 or POS 02 depending on payer rules).
Documentation Requirements for Mental Health CPT Codes
Accurate documentation is the difference between clean claims and chaotic billing. For CPT codes to be accepted, providers must document:
- session duration that matches the CPT code
- treatment goals and progress
- therapeutic interventions used
- patient response during the session
- time spent face-to-face
- diagnosis linking the service to medical necessity
Most denials occur because documentation and CPT codes don’t align. Insurers compare time notes with the CPT code automatically.
Avoiding Common Errors With Mental Health CPT Codes
Billing issues in mental health almost always tie back to avoidable mistakes. The most common errors include:
- using psychotherapy codes for medication-only visits
- mismatching session times
- skipping telehealth modifiers
- using outdated CPT codes
- incorrect combination of E/M and psychotherapy codes
- missing add-on codes
- documentation not supporting the service billed
Clean claims depend on precision. One inaccurate CPT code can lead to immediate denial or major reimbursement delays.
How Mastery of CPT Codes Improves Reimbursement
When practices apply mental health CPT codes correctly, their entire revenue cycle stabilizes. Insurance companies process claims faster, denial rates drop, and reimbursements become predictable. Accurate CPT coding directly improves:
- monthly cashflow
- first-pass claim acceptance
- reduced administrative workload
- compliance protection
- long-term financial growth
Mastery of mental health CPT codes isn’t optional it’s a financial necessity.
Conclusion: Correct Mental Health CPT Codes Secure Your Revenue
Mental health CPT codes determine how much a practice earns, how fast claims are paid, and how consistent reimbursements remain. If a private practice wants a stable revenue cycle, clean claims, and minimal denials, it must use correct CPT codes, maintain proper documentation, and follow payer-specific guidelines. Precision in mental health CPT coding isn’t just good practice it’s the foundation of long-term financial success.